Office Hours
518-383-5595
| Monday |
|---|
| 7:45am - 6:00pm |
| Tuesday |
| By Appointment |
| Wednesday |
| 7:45am - 6:00pm |
| Thursday |
| 7:45am - 6:00pm |
| Friday |
| By Appointment |
| Saturday & Sunday |
| Closed |
Appointment Request
Welcome to Ferguson Family Chiropractic, PLLC!
Families throughout the Capital Region choose Dr. John Ferguson for their pediatric and family wellness needs.
Steps to a healthier family:
1. Call our office 518.383.5595 or
fill in an appointment request form here.
2. Come in for your complimentary consultation.
3. Walk away with steps on how to improve your health concerns.
We are the Capital Region's Experts in helping children to overcome sensory and motor issues due to nerve system stress. We help your CHILD achieve the WELLNESS and FUNCTION they DESERVE!
Dr. John supports and is a member of the International Chiropractic Pediatric Association. A great resource for health-conscious parents. Visit them on the web:
https://icpa4kids.org
Health Articles

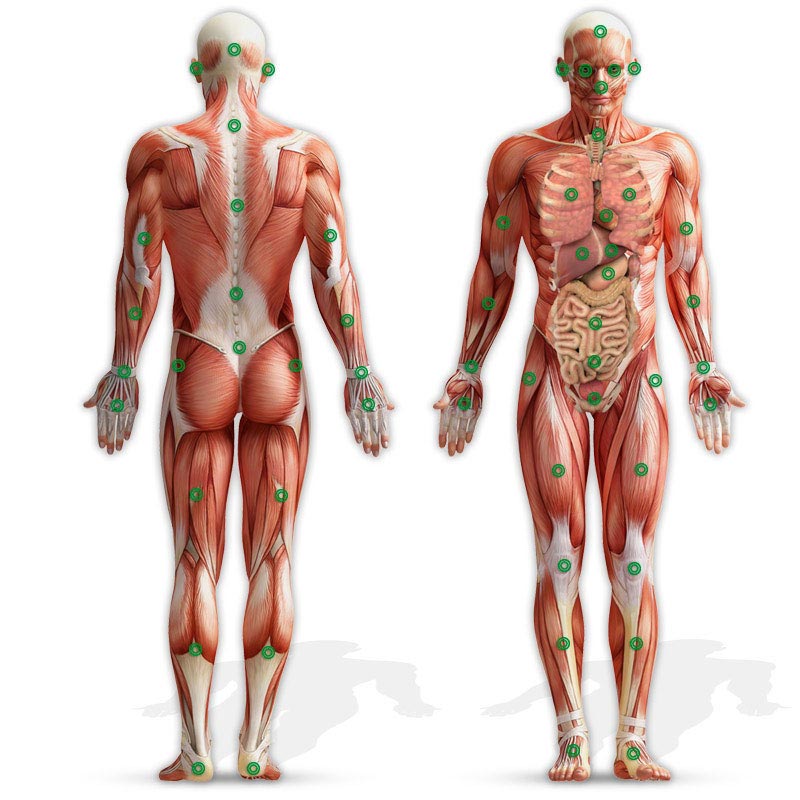
Automobile accidents are a common occurrence. The National Law Review ran an article on January 26, 2021, by attorney Richard P. Console, Jr. that stated, "Rear-end accidents are among the most common types of car accidents. They are also very dangerous. These accidents occur most often while one vehicle . . .
Read More
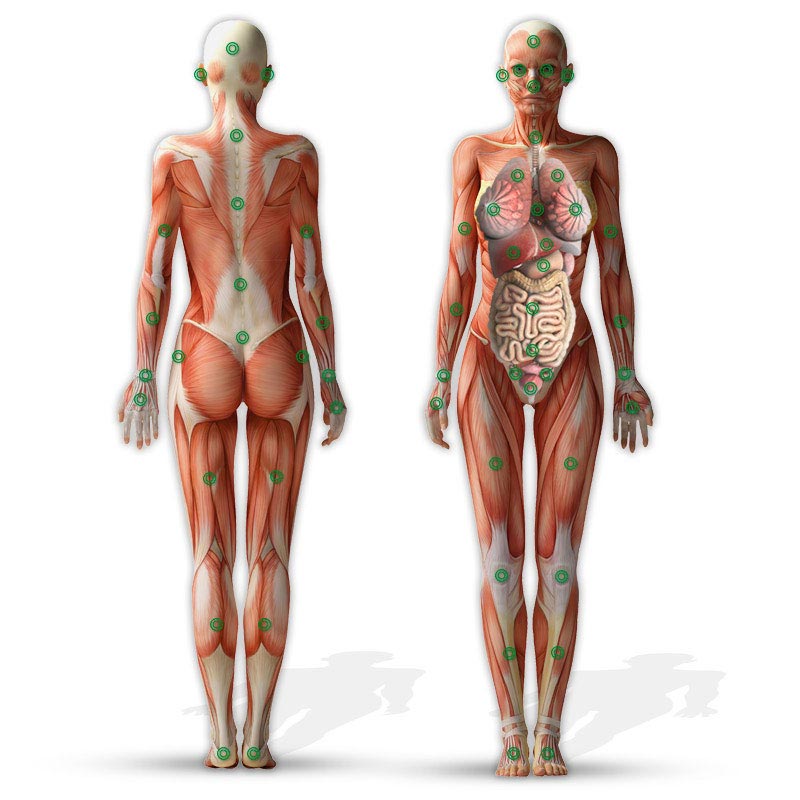
Menstrual Cycle Problems and Infertility Helped by Chiropractic
The Asian-Pacific Chiropractic Journal published the results of a case study in their third-quarter 2023 edition that documented a case of a woman suffering with menstrual cycle problems and infertility who was helped by chiropractic. . . .
Read More
Tonsillitis Resolved Under Chiropractic Care
The Journal of Upper Cervical Chiropractic Research released the results of a case study on February 1, 2024, documenting the resolution of enlarged tonsils on a pediatric patient receiving chiropractic care. According to the National Library of Medicine’s National Center for Biotechnology Information, . . .
Read More
Sleep Apnea Helped by Chiropractic Care and Nutritional Changes
On June 22, 2023, the Journal of Chiropractic Medicine published the results of a case study showing that chiropractic care, in conjunction with dietary changes, significantly helped a patient who was suffering with severe sleep apnea. . . .
Read More